The PT, OT, and SH Association Presidents regularly meet with DHS and AFMC to discuss issues that providers have when requesting Prior Authorizations (PAs) for children who need therapy over the 90-minute cap. These are the results of their latest meeting.
Keep track of your questions and email them to be discussed at the next meeting.
The Recap of ArkSHA, ArPTA, and AROTA meeting with AFMC and DDS on 08-25-17:
The following are issues raised by members of ArkSHA, ArPTA and AROTA, and responses from AFMC and DDS.
Issue: Shifting of Units Between Therapist and Assistant
There are still questions regarding the length of time it is taking to shift units from PT/OT/ST to PTA/COTA/SLPA and vice versa. AFMC reports that following completion of the large number of DMS-640 form validations AFMC received many change requests to prior authorizations. AFMC encouraged their staff to continue to process initial DMS-640 validations and that all changes would need to be checked before processing. Currently, AFMC states that they are about 10 days out on corrections and Jarrod McClain, AFMC Director for Clinical Review, indicated that their staff are working diligently to get the updates made as quickly as possible. The updates to the PA’s flow to DXC each night and providers can start billing immediately upon receipt of the changes.
In addition, Jarrod stated that AFMC is working to decrease the timeframe for corrections but they have to ensure that they are getting the correct request ID modified. According to Jarrod, it takes a few days to check and update the claims data extract file. If providers continue to see a delay, please contact Jarrod McClain at AFMC. He will personally see that his staff checks on the status of their request and get it processed.
Issue: Use of evaluations from preschool programs to kindergarten
There was concern from many members as to how long their evaluations will be valid in a schools setting. The consensus is that if the evaluation utilized is an evaluation conducted by a non-educational agency, or by a provider who is not contracted by an educational agency, then the evaluation is good for one year. If an educational agency or a contractor of the educational agency conducted the evaluation, then the evaluation falls under the school-based evaluation criteria of every 3 years.
Issue: Some prior authorizations were only approved after sending in a cover sheet restating information included in the evaluation.
AFMC was aware of this issue and is working to improve their processes for approval. In the meantime, providers are encouraged to highlight justification for medical necessity in the evaluative reports, including statements about how the services recommended are under accepted standards of practice to treat the patient’s condition, how services are complex and will require the skilled services of a qualified therapist, and a statement about therapy prognosis (See Medicaid Manual Section II). Though a cover letter outlining these justifications is not required, providers are encouraged to consider using a cover letter attached to the evaluation to make these medical necessity statements more salient for reviewers.
Issue: Are reviewers actually reading the evaluations or just looking for technical language?
AFMC assured us that they are reading all evaluations. They perform both technical and administrative reviews in order to ensure that all requirements of the evaluative reports are included, as well as a medical necessity review to ensure that justification for medically based services is included.
Issue: I heard that AFMC was using nurse reviewers and not experienced pediatric therapists in each discipline. Is this true?
AFMC utilizes registered nurses to perform the initial reviews of all PA requests. If a request is denied than the request is assessed by an experienced licensed therapists specific to the discipline. If the therapist agrees with the denial it is then sent to a board certified pediatric physician for final review. If a provider does not agree with the denial or would like to request reconsideration they may do so by resubmitting the request.
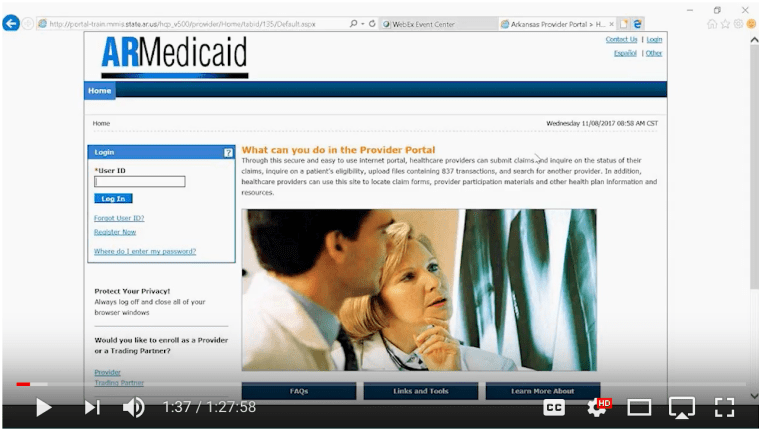
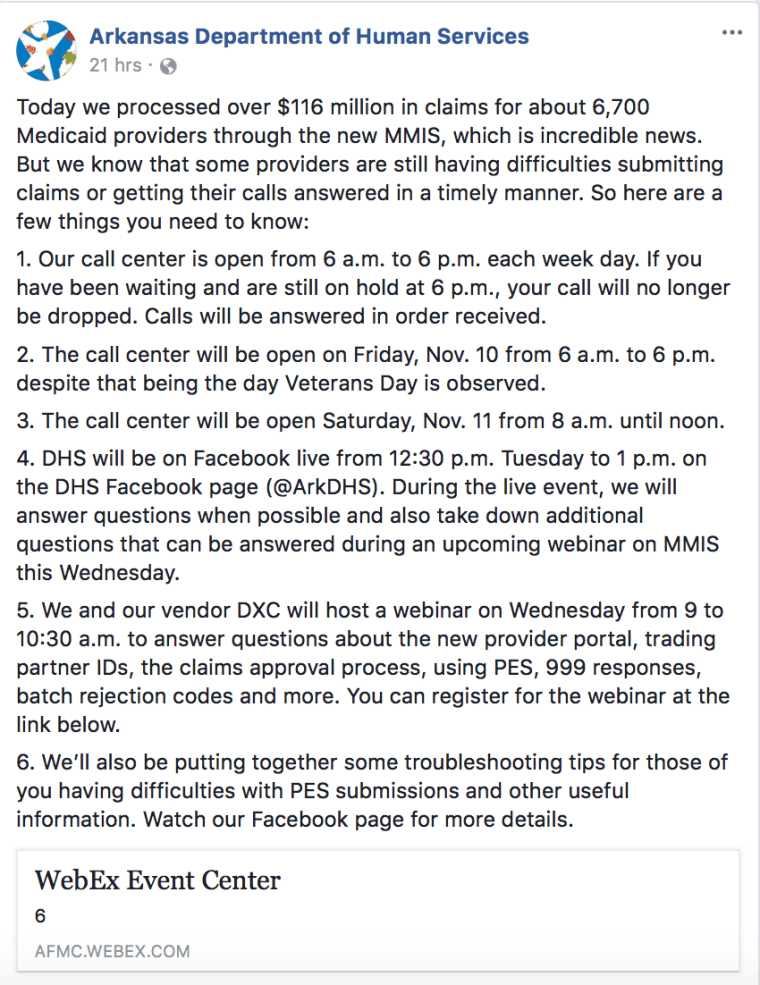
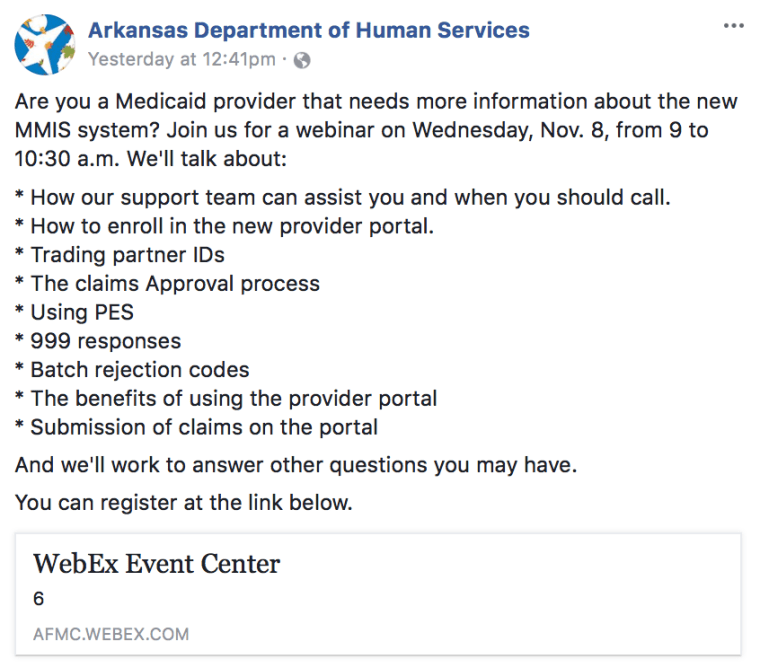
Issue: What about beneficiaries who receive services from multiple providers for the same service?
AFMC and DDS continue to emphasize the need for care coordination for beneficiaries with multiple providers of the same modality (physical, occupational or speech therapy). Dr. Chad Rodgers, AFMC Medical Director, attended our meeting and reported that the pediatricians and PCPs he has been in contact with are interested in understanding what situations justify the appropriate signing off on multiple prescriptions. He asserts that although he can’t speak for all physicians he personally looks at every request for therapy services before signing them. He recognized that it is difficult to for most physicians to understand why a child needs multiple services. He and assistant director of DDS Elizabeth Pittman stated that it would be beneficial to state on the DMS-640 the specific need for a particular service and that the beneficiary will need the services of multiple therapists. AFMC and DDS are considering a change to the DMS-640 forms in the future to accommodate the different services provided within one discipline. Elizabeth Pittman reported that the new MMIS system (which has an anticipated implementation of summer of 2018) will be less burdensome on providers and will have the ability to disclose is the beneficiary is receiving services from other providers. Until then, providers need to ask during the intake process if the recipient is receiving therapy services from any other provider, and then coordinate as needed. According to Jarrod McClain, only 10 providers have bumped into challenges with the multiple provider issues thus far.
Issue: For short term scripts (i.e. ortho docs who write for 2-6 weeks) that then need an extension once the patient has had a follow-up recheck. What is the most efficient way to keep PA’s from having to be unnecessarily done?
Providers can simply go into Review Point, and click the extend button. The codes will be transferred over and the new prescription can be uploaded. Information about the progress of the patient and continued medical necessity should be included with the extension.
Issue: It has come to the attention of AFMC and DDS that some facilities are sending notices to parents that they should not allow services for their child in the school due to the need for a PA if the school and independent facility are both treating the beneficiary.
Although Medicaid is a “medical” assistance program, it recognizes the importance of school-based services. The federal Medicaid program actually encourages states to use funds from their Medicaid program to help pay for certain healthcare services that are delivered in the schools, providing that federal regulations are followed. The associations stand with AFMC and DDS that sending notices to parents regarding billing for services between schools and independent clinics is not recommended. IDEA laws require schools to provide services to beneficiaries if needed for educational purposes. Schools also must provide therapy that is medically necessary. Therapy services outside of the school setting should not replicate services provided by therapists contracted or working with the school.
Issue: A representative at DHS has stated that physical therapy re-eval codes are no longer a valid code as of July 1st. Has anything changed in the recent rule change?
Reevaluation codes are not currently and haven’t been a reimbursable code. The two billable codes for physical therapy services are 97001 and 97110.